Themen dieses Blogartikels:
Table of contents
- Do you know how vitamin D regulates your immune system?
- What is vitamin D anyway?
- What are the important functions of vitamin D in the body?
- Vitamin D and bones
- Vitamin D and cell division
- Vitamin D and the immune system
- Why are sunlight and food alone not enough?
- When is the vitamin D receptor possibly reduced?
- The vitamin D ratio - has your doctor already explained this to you?
- It all depends on the right ratio
- Always have the vitamin D ratio checked before supplementation
- Vitamin D supplementation - how to do it right
- The BODI protocol
- Sources & bibliography
Do you know how vitamin D regulates your immune system?
“Vitamin D deficiency is not as rare as you might think. Vitamin D intake is particularly important during the winter months to prevent symptoms such as reduced bone stability and immune deficiency. I test the vitamin D levels of every patient who comes to my practice. My motto is “measure, do, measure.”
- Christian Burghardt
Around 60% of all adults in Germany have a vitamin D deficiency or are insufficiently supplied with it1. The rate is estimated to be higher among older people. But does a lot of vitamin D help a lot? In this article, we explain the special immune vitamin D. What exactly is it, what can it do and how can you benefit from vitamin D?

What is vitamin D anyway?
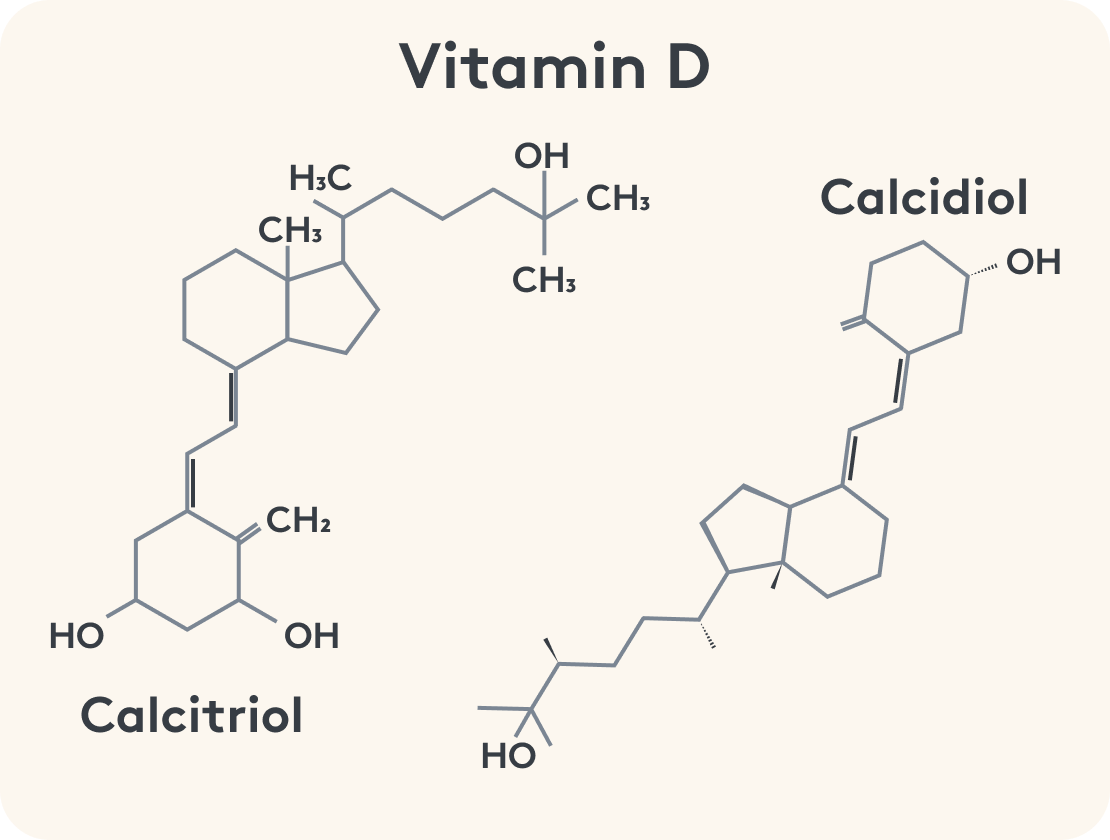
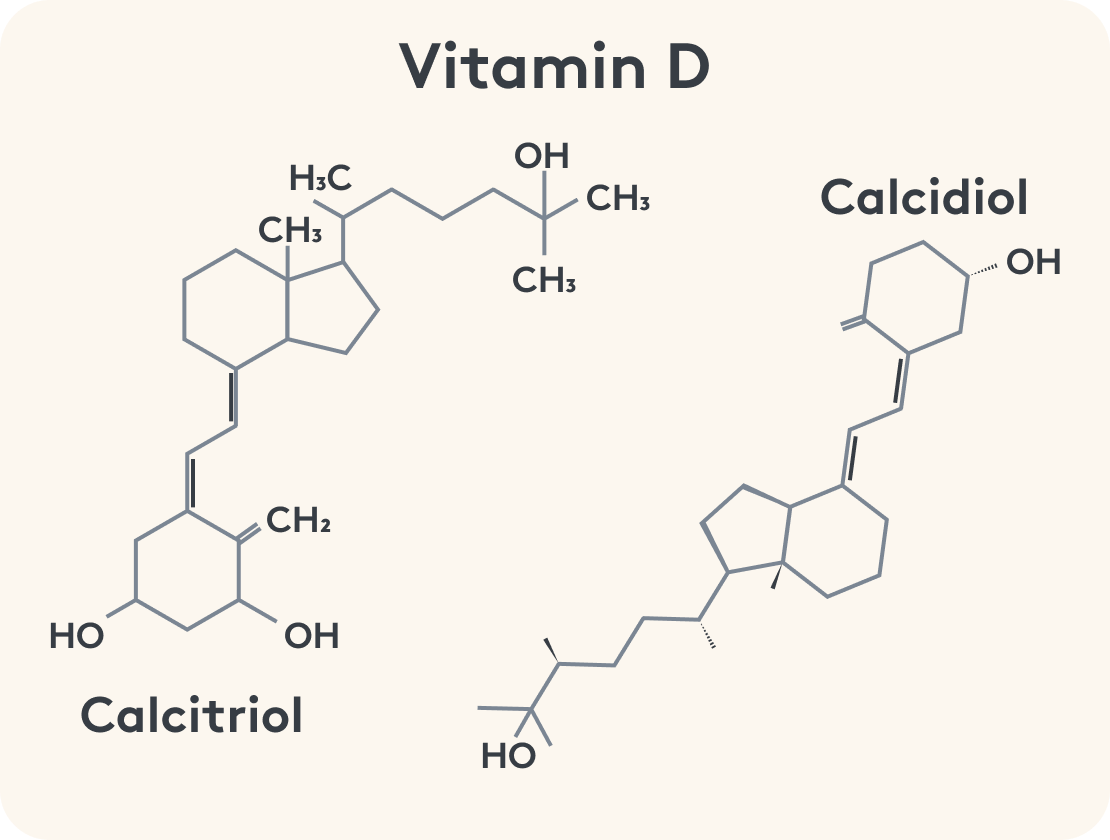
Vitamin D is a fat-soluble vitamin and belongs to the group of fat-soluble vitamins, together with vitamins A, E and K. Another name for the group of D vitamins is cholecalciferols or calciols. There is actually more than just one vitamin D. The hormonally active form is calcitriol (1,25-dihydroxycholecalciferol), while the direct precursor is calcidiol (25-hydroxycholecalciferol). The conversion step is the regulating step of vitamin D metabolism. Vitamin D is now also referred to as a hormone - as it can theoretically be produced independently by the body. This requires UV-B radiation from the sun.
What are the important functions of vitamin D in the body?
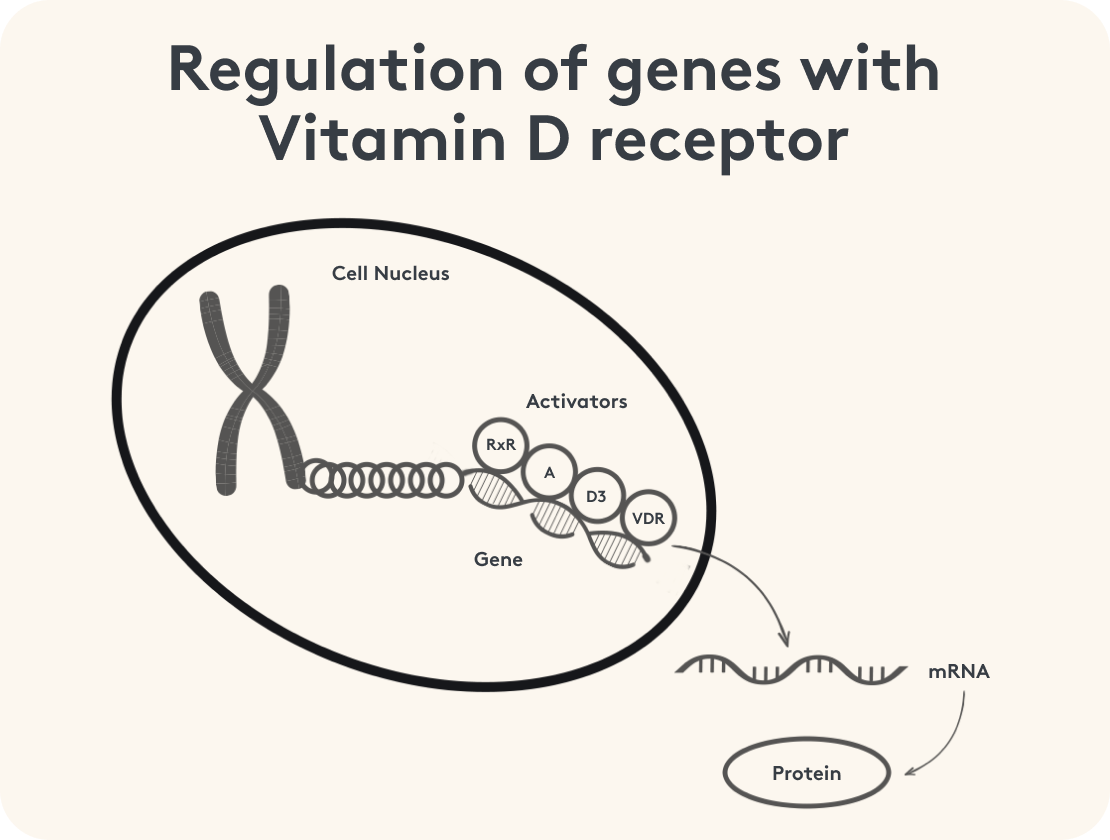
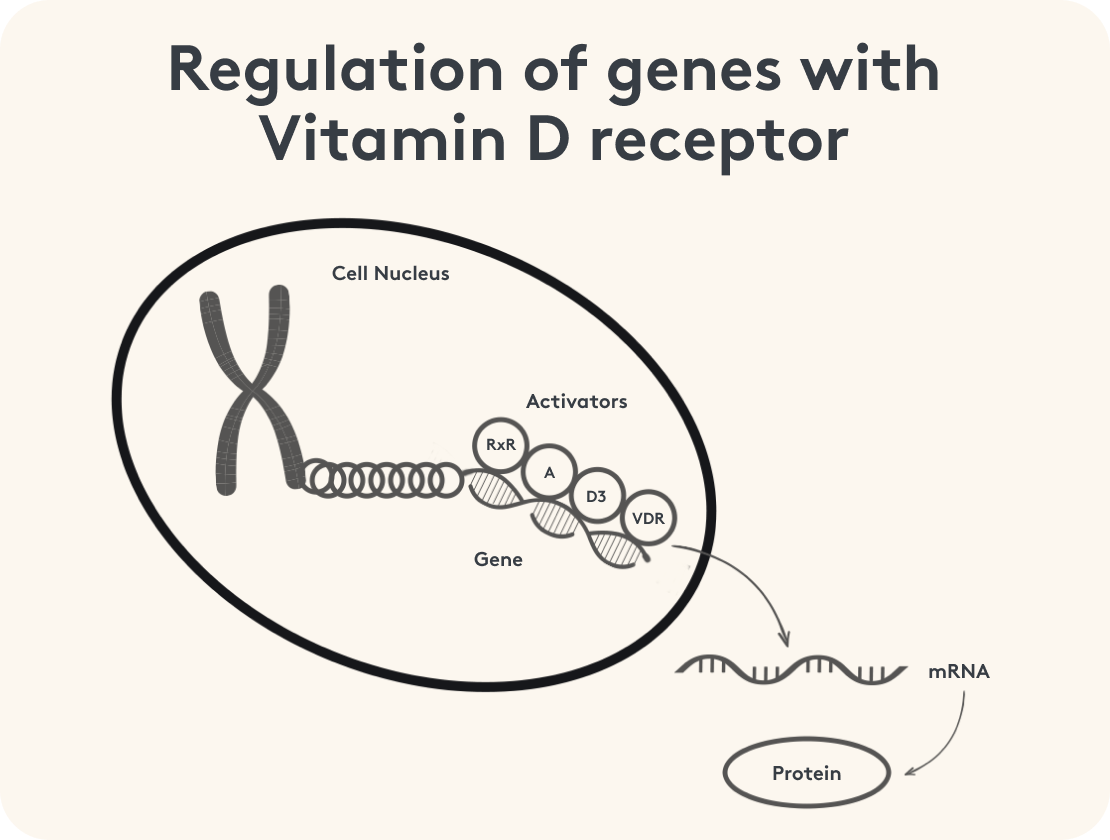
When used correctly, vitamin D performs many functions in your body. Did you know that vitamin D can even regulate your genes and therefore influence how your cells' metabolism and processes work? An adequate supply of vitamin D is therefore essential for good health.
Let's start from the beginning.
Vitamin D and bones
The bone-preserving function of the vitamin is particularly well known. Together with calcium, magnesium and boron, vitamin D contributes to the bone balance. It can promote bone storage. For a long time, this function of the vitamin was the only one generally known. Vitamin D was limited to the bone balance. Even today, classical medical students mainly learn about this function. In this article, we therefore want to look at the other functions of vitamin D and show what else vitamin D can do. It is also important to monitor vitamin D levels to ensure that they are adequate, especially for bone health.
Vitamin D and cell division
Let's start with cell division. Cell division is important for cells to ensure that new, healthy cells are created and that the tissue is maintained. A growth and division process that is too fast is just as problematic as one that is too slow. If the cells divide more frequently, the resulting daughter cells are statistically more likely to mutate, as the mother cell has not taken the time to check the DNA that has been created. Vitamin D contributes to the regulation of cell division and thus also prevents excessive proliferation (= cell division and growth).
Vitamin D and the immune system
Vitamin D3 is extremely relevant in the context of the immune system. However, the effect of vitamin D3 on your immune system cannot be generalized. Vitamin D has a lot of potential, especially via gene regulation. Some of the points of attack of vitamin D on the immune system are
- A boost to the innate immune system by activating macrophages (phagocytes) and natural killer cells²
- Increased formation of antimicrobial peptides (AMP); these help to keep the concentration of the pathogen low, especially in the initial phase³
- Vitamin D stimulates anti-inflammatory messenger substances and hinders pro-inflammatory pathways; inflammation is thus reduced⁴
- Regulatory T cells are promoted, while other cells of the acquired immune system tend to be inhibited in their activity or become more tolerant⁵
Broadly speaking, vitamin D strengthens the immune system in terms of immediate defense (killing) and regulation of the immune response so that it does not overshoot and degenerate into inflammation or an autoimmune process. At the same time, vitamin D reduces the activity of the acquired immune system.
Why are sunlight and food alone not enough?
You've probably heard this recommendation before: “Half an hour in the sun is enough to cover your vitamin D requirements for the day.” Why do they say that? And is it true?
Vitamin D is a special vitamin. Unlike other vitamins, you can produce vitamin D yourself. The inactive precursor is converted into the active stage with the help of sunlight (UV-B radiation).
However, in our latitudes in particular, the angle of sunlight is quite low - even in summer. According to the DGE (German Society for Nutrition), in order to produce enough vitamin D in this country, a fair-skinned person should stand in the sun for 10 minutes at midday (between 12 and 3 p.m.) in summer, leaving a quarter of the body surface uncovered. In spring and early fall it is up to 20 minutes. If you are dark-skinned, the time is longer as the sun's rays do not penetrate the skin as well. In late fall and winter, it is not possible to cover the daily requirement with sunlight as it is not strong enough⁶.
This ability is also dependent on the use of sun creams. Although sunscreen & co. protect against sunburn, skin changes and even cancer, they inhibit the production of vitamin D by blocking UV-B radiation. The levels achieved by following the DGE instructions are nevertheless in the lower normal range, if at all. It is not for nothing that only around 38% of adults achieve sufficient vitamin D levels1. It is therefore important to discuss your vitamin D intake with a doctor in order to avoid an undersupply.
The vitamin D content in food is very limited. Fish, eggs, mushrooms and liver contain small amounts of vitamin D. Herring is the best source here. So you can't necessarily count on getting it from food.
Another possible problem with the body's own synthesis or absorption through food is the availability of the vitamin D receptor, which is limited in many individuals.
The vitamin D receptor is a protein to which vitamin D binds in the cell. Only with this receptor can vitamin D have its effect on your genes and thus cause the above effects6. If this receptor is missing, there are problems with vitamin D metabolism, as unbound, active vitamin D in your cell can even have negative effects by further inhibiting the production of the vitamin D receptor and promoting inflammation⁷.
Now you know: The vitamin D receptor is important for vitamin D to perform its positive functions. Without the receptor, vitamin D intake can even backfire completely. How do you know when your vitamin D receptor is not being produced enough?
Advertisement
Comprehensive supply of all fat-soluble vitamins A, D, E & K
Enhanced formula with vitamin K1+ K2 in a 1:1 ratio & excellent bioavailability
Vegetarian & free from gluten & lactose
Combined with valuable coconut & olive oil for optimal absorption
No fillers or additives
Developed in collaboration with doctors & experts

When is the vitamin D receptor possibly reduced?
Many factors influence the vitamin D receptor. A few of the causes are:
- Some pathogens use the reduction of the vitamin D receptor as a means to survive⁸
- An excess of active, unbound vitamin D3 (1,25(OH)2)
- Proinflammatory cytokines, i.e. messenger substances that promote inflammation⁹
- Nitrosative stress¹⁰
- Calcium deficiency, as it leads to an increased level of active vitamin D3
So you can remember: The vitamin D receptor is inhibited, especially in the case of inflammation & pro-inflammatory messengers, and cannot perform its function. These inflammations lead to more active, unbound vitamin D3 and this in turn leads to fewer vitamin D receptors.
How can you specifically recognize whether your vitamin D receptor has problems?
The vitamin D ratio - has your doctor already explained this to you?
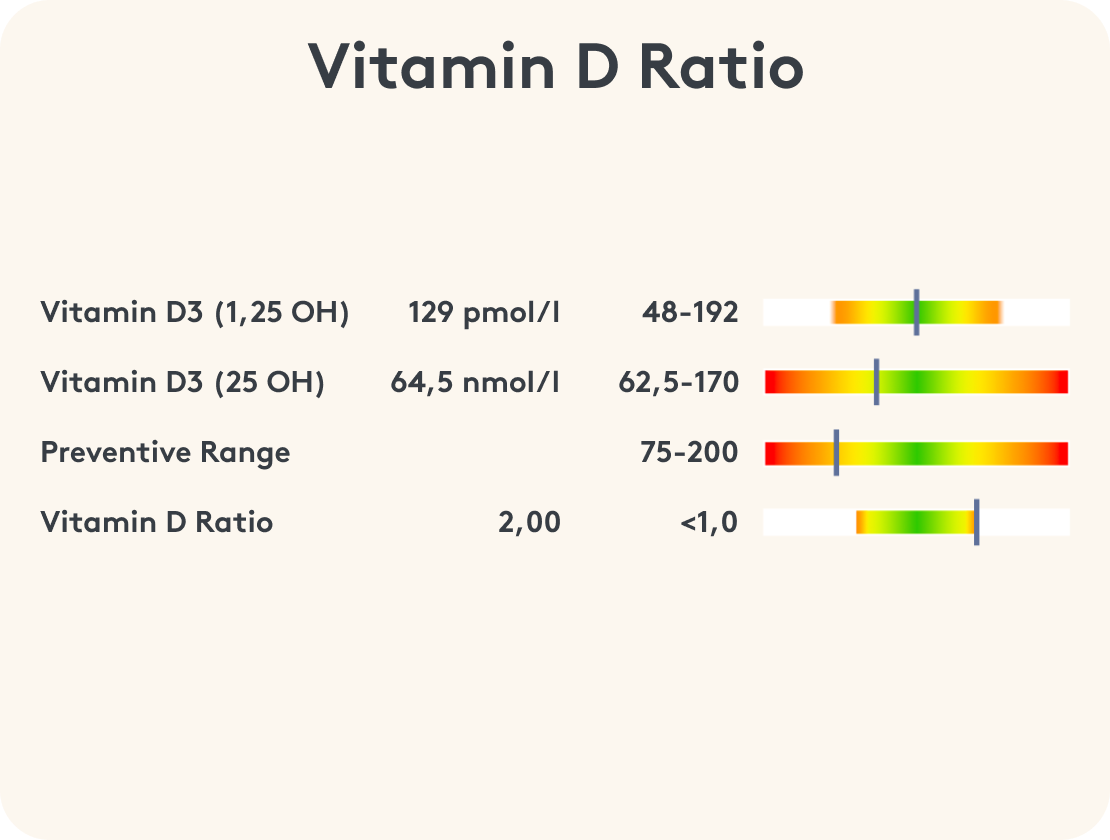
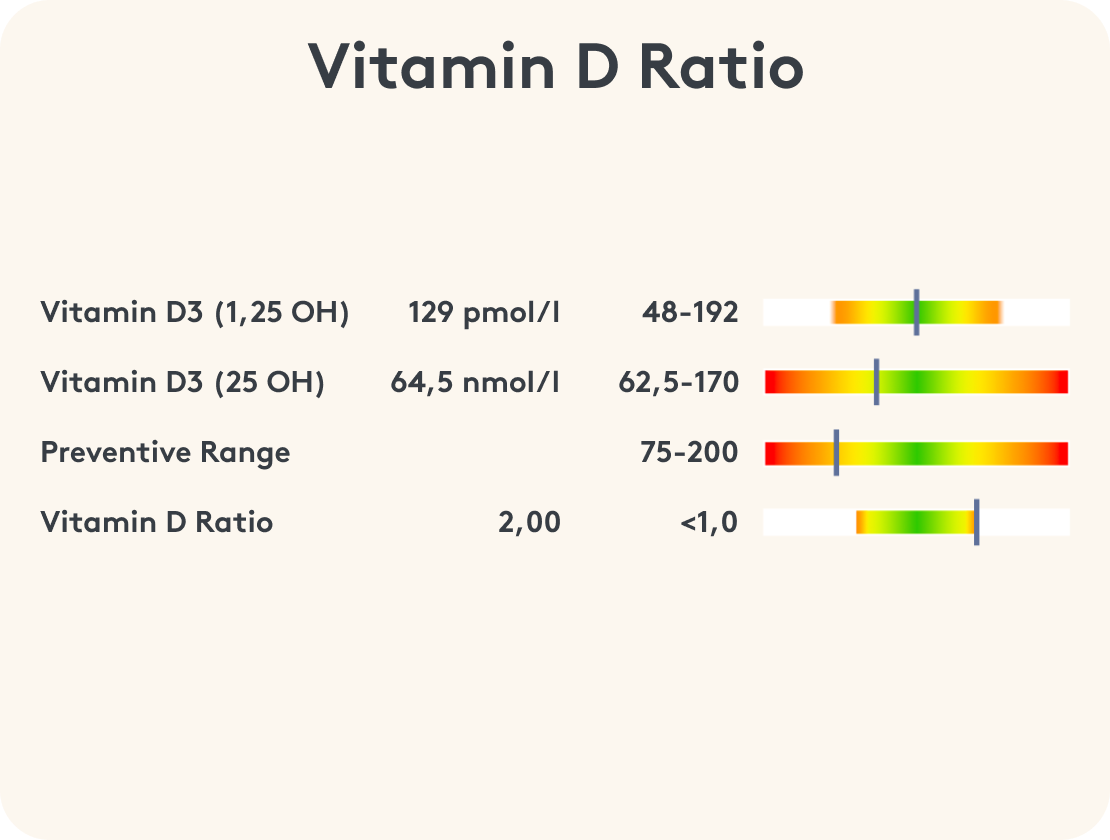
If there is a problem with the vitamin D receptor, the level of active vitamin D3 (1,25(OH)2) is usually elevated. With the normal vitamin D value, however, your doctor only measures the direct precursor: inactive 25(OH) vitamin D. The value can even be lowered if there is a problem with the utilization of vitamin D, because the precursor is increasingly converted to active vitamin D3 in the case of inflammation and vitamin D receptor deficiency.
If only the inactive 25(OH) vitamin D value is measured in your case, your doctor cannot say whether you have a vitamin D deficiency or a vitamin D receptor deficiency.
Show your doctor the following article. Maybe they will even decide to measure the ratio more often in the future before giving vitamin D blindly. Just like the well-known principle: "measure, do, measure".
Advertisment
Complex of vitamin D3 with factors such as natural vitamin K2 (as MK-7-all-trans), natural calcium from sango sea coral, bioactive magnesium as glycerophosphate, natural silicon from bamboo extract & boron
Synergy complex focus on optimized bioavailability
No fillers or additives
Developed with doctors & experts

It all depends on the right ratio
This is where the importance of the vitamin D ratio comes in. It enables a more precise assessment by measuring both active 1,25(OH)2 vitamin D3 and inactive 25(OH) vitamin D and comparing them. An elevated ratio - i.e. a vitamin D ratio above 1 - indicates possible disorders, such as a vitamin D receptor deficiency or a chronic inflammatory disease. Interestingly, studies such as that by Chung et al. (2011)12 show that while low 25(OH) vitamin D levels correlate with an increased risk of chronic diseases such as autoimmune diseases or cardiovascular problems, simply increasing 25(OH) vitamin D does not provide any significant clinical benefit in people who are already ill. Autier et al. (2014)13 also came to the conclusion that low 25(OH)D levels are often associated with chronic inflammation, but that forced administration of 25(OH)D had no therapeutic effect on affected patients. On the contrary: in some inflammatory diseases, the increased conversion of 25(OH)D to active 1,25(OH)2 vitamin D3 even leads to proinflammatory effects.
Always have the vitamin D ratio checked before supplementation
A ratio above 1 could indicate an excessive production of 1,25(OH)2 vitamin D3, which can intensify inflammatory processes. In such cases, additional administration of vitamin D would even be counterproductive. A ratio of less than 1 would be optimal in order to ensure a balance between the vitamin D forms and minimize the risk of undesirable pro-inflammatory reactions. Feel free to show your doctor the article linked below. Perhaps they will decide to measure the ratio more often in future before blindly prescribing vitamin D - according to the well-known principle: “measure, do, measure”.
Vitamin D supplementation - how to do it right
You may be thinking to yourself now: What can I do if I am one of those people who have problems with the vitamin D receptor? Can I still take vitamin D? Do I have to pay attention to anything? How can I get rid of the receptor problem?
Good news: You can solve the problem with your vitamin D receptor and ensure that your vitamin D metabolism works properly!
This is where the vitamin D binding protein (VDBP) comes into play. This protein can bind vitamin D in a similar way to the vitamin D receptor and thus replace it¹¹. This allows vitamin D to perform its actual functions again and strengthen or modulate the immune system.
And the best thing is that because we have less free, active vitamin D3, the vitamin D receptor is less inhibited and you gradually return to a normal state.
To ensure that the vitamin D can be utilized, a few cofactors are also relevant:
- The minerals magnesium, calcium and boron, as well as vitamin K2 are cofactors, especially in bone metabolism; a calcium deficiency promotes inhibition of the vitamin D receptor
- Vitamin A (retinoic acid | retinol) is involved in gene activation together with its receptor, the RXR
- In the event of inflammation, you must of course also work with your doctor to counteract this so that your vitamin D metabolism is restored more quickly.
Let's summarize again: For a good vitamin D metabolism, which is important for regulating the immune system and cell division, among other things, you need a functioning vitamin D receptor. If this is inhibited, you can work with vitamin D-binding proteins as a substitute and also support its utilization with the cofactors magnesium, calcium and boron, as well as vitamin A and K2. If you have inflammation, you should also make sure you stop it. It is also important to reduce the risk of vitamin D deficiency in order to avoid symptoms such as decreasing bone stability and immune deficiency.
The BODI protocol
This is basically how the BODI protocol came about. The cofactors, the vitamin D-binding protein, the support of the immune system and of course vitamin D itself were important to the Munich doctor Christian Burghardt. He realized years ago that although his patients had a vitamin D deficiency and inflammatory processes, the administration of vitamin D alone did not improve vitamin D levels and inflammation parameters. The BODI protocol, named after the practice of our MITOcare founders Christian Burghardt and Dr. Alexander Hierl, combines these findings with the results of current research.
The BODI protocol, named after Christian Burghardt's practice of the same name, combines these insights with the results of current research.
"With a moderate vitamin D dose of 2,000 IU and the cofactors, I have achieved much more with my patients than with a high vitamin D dose alone of, for example, 20,000 IU. The BODI protocol is used daily for me to address the vitamin D problem well. I can't imagine life without it."
- Christian Burghardt, Head of BODI (Burn Out Diagnostic Institute)

Knowledge transfer to our MITO partners
With our MITOcare Academy for specialist users, we pass on our knowledge of functional medicine, micronutrients and complex physical relationships to our MITO partners. We hope that as many doctors, alternative practitioners and other specialist users as possible will gain comprehensive knowledge and thus be able to help everyone achieve their best possible balance.
If you would like to have your vitamin D ratio checked, please contact the doctor or alternative practitioner you trust and show them the above-mentioned specialist article. Would you like to get in touch with our MITO partners? Our customer service will be happy to help you.
This article is based on carefully researched sources:
Sources & bibliography
- Rabenberg, M., Mensink, GBM (2016). Vitamin D status in Germany, 1(2), 36-42. edoc.rki.de/handle/176904/2492
- Bikle DD (2009). Vitamin D and immune function: understanding common pathways. Current osteoporosis reports, 7(2), 58–63. doi.org/10.1007/s11914-009-0011-6
- Gombart AF (2009). The vitamin D-antimicrobial peptide pathway and its role in protection against infection. Future microbiology, 4(9), 1151–1165. doi.org/10.2217/fmb.09.87
- Chen, Y., Liu, W., Sun, T., Huang, Y., Wang, Y., Deb, DK, Yoon, D., Kong, J., Thadhani, R., & Li, YC (2013). 1,25-Dihydroxyvitamin D promotes negative feedback regulation of TLR signaling via targeting microRNA-155-SOCS1 in macrophages. Journal of immunology (Baltimore, Md. : 1950), 190(7), 3687-3695. doi.org/10.4049/jimmunol.1203273
- Peelen, E., Knippenberg, S., Muris, AH, Thewissen, M., Smolders, J., Tervaert, JW, Hupperts, R., & Damoiseaux, J. (2011). Effects of vitamin D on the peripheral adaptive immune system: a review. Autoimmunity reviews, 10(12), 733-743. doi.org/10.1016/j.autrev.2011.05.002
- Mayne, CG, Spanier, JA, Relland, LM, Williams, CB, & Hayes, CE (2011). 1,25-Dihydroxyvitamin D3 acts directly on the T lymphocyte vitamin D receptor to inhibit experimental autoimmune encephalomyelitis. European journal of immunology, 41(3), 822-832. doi.org/10.1002/eji.201040632
- Mangin, M., Sinha, R., & Fincher, K. (2014). Inflammation and vitamin D: the infection connection. Inflammation research : official journal of the European Histamine Research Society ... [et al.], 63(10), 803–819. doi.org/10.1007/s00011-014-0755-z
- Yenamandra, S.P., Lundin, A., Arulampalam, V., Yurchenko, M., Pettersson, S., Klein, G., & Kashuba, E. (2009). Expression profile of nuclear receptors upon Epstein -- Barr virus induced B cell transformation. Experimental oncology, 31(2), 92–96
- Mayur, N., Lewis, S., Catherwood, BD and Nanes, MS (1993), Tumor necrosis factor α decreases 1,25-dihydroxyvitamin D3 receptors in osteoblastic ROS 17/2.8 cells. J Bone Miner Res, 8: 997-1003. doi.org/10.1002/jbmr.5650080813
- García-Barragán, Á., Gutiérrez-Pabello, JA, & Alfonseca-Silva, E. (2018). Calcitriol increases nitric oxide production and modulates microbicidal capacity against Mycobacterium bovis in bovine macrophages. Comparative immunology, microbiology and infectious diseases, 59, 17–23. doi.org/10.1016/j.cimid.2018.09.001
- Kongsbak, M., von Essen, MR, Levring, TB, Schjerling, P., Woetmann, A., Ødum, N., Bonefeld, CM, & Geisler, C. (2014). Vitamin D-binding protein controls T cell responses to vitamin D. BMC immunology, 15, 35. doi.org/10.1186/s12865-014-0035-2
- Chung, M., Jounghee L., Terasawa, T., Lau, J., Trikalonos, TA (2011). Vitamin D with or without calcium supplementation for prevention of cancer and fractures: an updated meta-analysis for the US Preventive Services Task, acpjournals.org/doi/10.7326/0003-4819-155-12-201112200-00005
- Autier, P., Boniol, M., Pizot, C., Mullie, P. (2014). Vitamin D status and ill health: a systematic review thelancet.com/journals/landia/article/PIIS2213-8587(13)70165-7/abstract