Themen dieses Blogartikels:
Table of Contents
- What are silent inflammations
- Definition and explanation of silent inflammation
- Difference to classic inflammations
- Causes of silent inflammation and inflammatory processes
- LPS as a trigger for inflammation
- Pro-inflammatory stimulus and immune balance
- How to recognize silent inflammation
- Parameters of the silent inflammation check
- hsCRP as a marker for silent inflammation
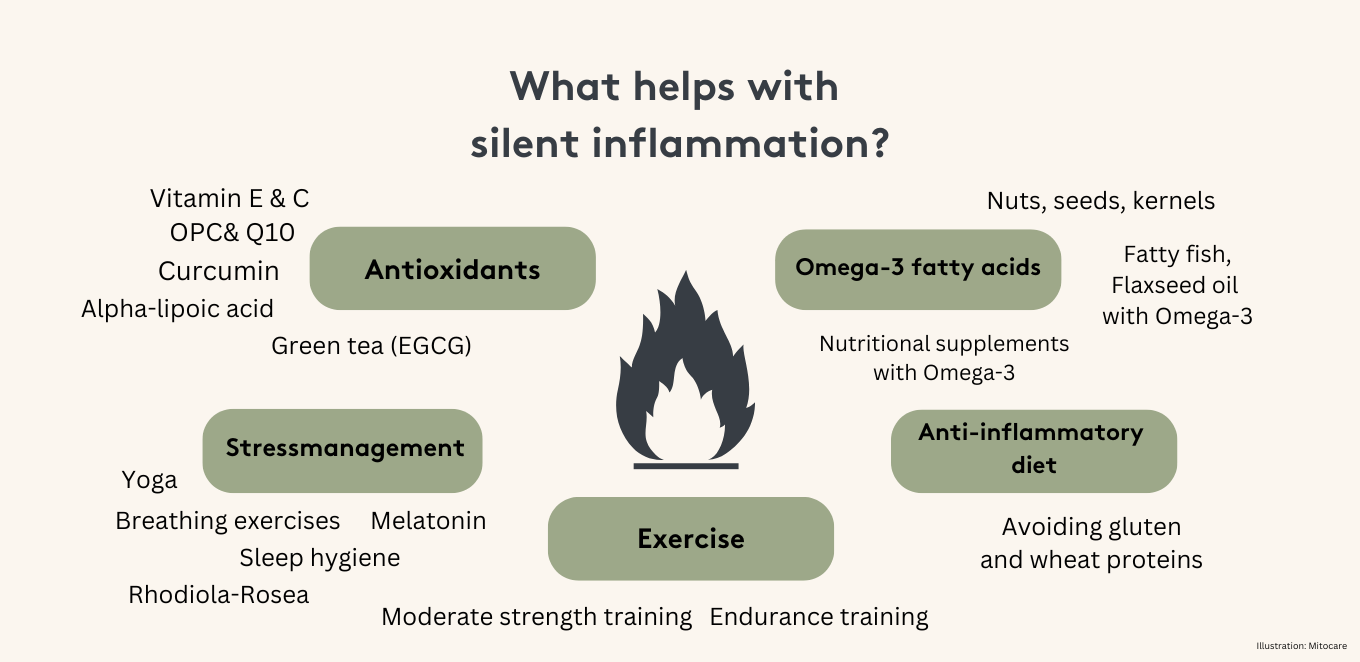
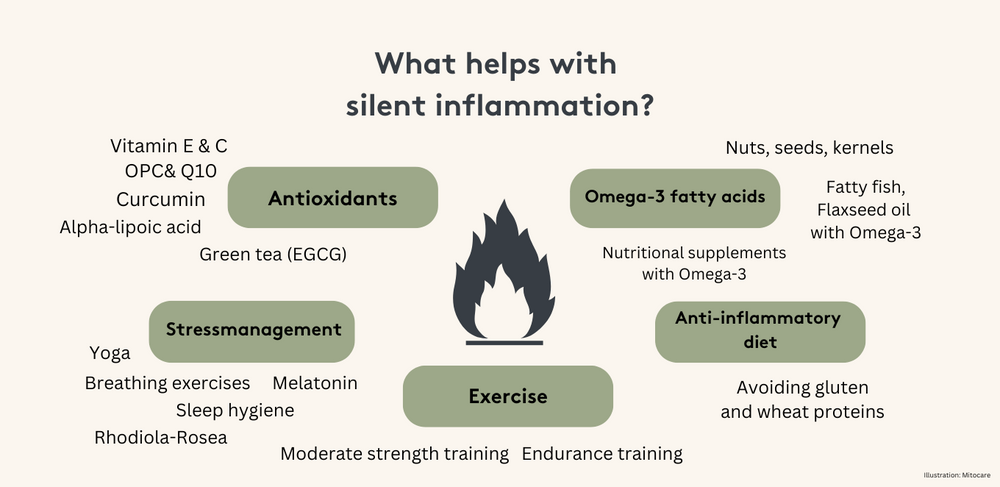
- Actions against silent inflammation
- Anti-inflammatory diet
- No wheat and gluten
- Stress management
- Movement
- Essential Oils
- Supplements
- Preventing inflammation - minimal effort, great benefit
- Bibliography
Inflammation is a natural reaction of the body to injuries or infections. It is a sign that the immune system is working and fighting harmful invaders. But what happens when your body is constantly in a state of inflammation without there being a visible cause? These processes, known as “silent inflammation”, often go unnoticed but can have serious health consequences. In this article, we look at what silent inflammation is, what causes it and how you can effectively counteract it.
What are silent inflammations
In contrast to acute inflammation, which is accompanied by pain, redness and swelling, silent inflammation is subliminal and often lasts for years. Your body reacts to certain stimuli with a chronic, low-grade inflammatory reaction. These inflammations often go undetected as they do not cause typical symptoms such as fever or pain. In the long term, however, they can damage tissue and increase the risk of diseases such as cardiovascular disease, diabetes, neurodegenerative diseases and even cancer1,2,3,4,5. In addition, silent inflammation can cause chronic muscle and joint pain, which underlines the importance of monitoring and treating such inflammatory processes.
Definition and explanation of silent inflammation
Silent inflammation, also known as silent inflammation, is a chronic, subclinical inflammation that can go unnoticed in the body. In contrast to acute inflammation, which is characterized by symptoms such as redness, swelling, pain and fever, silent inflammation often does not manifest itself through classic symptoms. Nevertheless, they can put a permanent strain on the immune system and the body and lead to secondary diseases such as cardiovascular disease, type 2 diabetes and depression⁶.
Silent inflammation can be triggered by various factors such as poor diet, too little exercise, stress⁷, sleep disorders⁸ and environmental toxins⁹. They can also be caused by foci of inflammation in the mouth and jaw system, such as untreated periodontitis.
The term “silent inflammation” was coined to refer to the fact that this type of inflammation often goes unnoticed until it leads to serious secondary diseases. It is therefore important to recognize and treat silent inflammation early in order to avoid long-term damage.
An important marker for silent inflammation is C-reactive protein (CRP), a protein that can be detected in blood plasma. An elevated CRP level can indicate silent inflammation. There are also other markers, such as high-sensitivity C-reactive protein (hsCRP), which is even more sensitive than normal CRP.
Treatment for silent inflammation usually involves a combination of dietary changes¹⁰, exercise¹¹ and targeted therapies to reduce inflammation and promote health. It is important that you work with a doctor or other health professional to find the best treatment for your specific situation.
Difference to classic inflammations
Silent inflammation differs from classic inflammation in many ways. While classic inflammations are characterized by clear symptoms such as redness, swelling, pain and fever, silent inflammations are often painless and go unnoticed. Classic inflammations are usually acute and occur as a direct reaction to injuries or infections. They subside after a certain time as soon as the healing process is complete.
In contrast, silent inflammations are chronic and can persist over a long period of time without you realizing it. These underlying inflammations can damage the tissue and lead to serious health problems in the long term. It is therefore important to recognize and treat silent inflammation at an early stage to avoid serious consequences.
Causes of silent inflammation and inflammatory processes
There are a number of factors that promote silent inflammation. Some of the most common causes are
- Unhealthy diet: sugar, refined carbohydrates and trans fats promote silent inflammation. Sugar causes rapid blood sugar fluctuations and increases insulin production, which intensifies inflammatory processes. In addition, food additives and contaminants found in processed foods can also trigger inflammatory reactions.
- Obesity and visceral fat: Adipose tissue, especially the so-called visceral fat around the organs, produces inflammation-promoting messenger substances. People with obesity are particularly at risk12,13 as excess body fat can trigger a chronic inflammatory reaction in the body. Certain nutritional supplements support the body in regenerating cells and, in combination with a healthy diet, can help to alleviate silent inflammation.
- Wheat proteins and gluten: Recent studies, in particular by Professor Detlef Schuppan, have shown that not only gluten, but also certain wheat proteins, such as the so-called amylase trypsin inhibitors (ATIs), can trigger immune reactions and promote silent inflammation. These proteins play a role in inflammatory diseases such as multiple sclerosis¹⁴, asthma¹⁵ and rheumatoid arthritis¹⁶. This could explain why many people who avoid gluten report a general relief of their inflammatory symptoms. Gluten-containing foods, especially those rich in ATIs, should therefore be avoided to reduce chronic inflammation.
- Chronic stress: Long-term stress leads to an increased release of the stress hormone cortisol. While cortisol has an anti-inflammatory effect in the short term, chronic release weakens the immune system and promotes silent inflammation. This can end in a dangerous cycle in which your body is permanently overloaded and the healing of inflammatory processes is disrupted.¹⁷ Relaxation techniques and a conscious approach to stress can help here.
- Lack of sleep: Chronic lack of sleep destabilizes the immune system and can increase inflammation in the body¹⁸. It's important to maintain a healthy sleep schedule to reduce silent inflammation. Studies show that even a single night of poor sleep can lead to an increase in pro-inflammatory cytokines. Therefore, you should consider sufficient sleep in combination with healthy sleep hygiene as an important factor in the fight against silent inflammation.
- Sleep disorders: Sleep disorders can be both a symptom and a cause of silent inflammation. A disturbed tryptophan metabolism can lead to a lack of serotonin, which promotes sleep disorders. Silent inflammation can also cause sudden sleep disturbances and fatigue.
- Lack of exercise: Regular exercise promotes fat burning and helps to reduce inflammatory processes in the body¹⁹. Even moderate exercise can have a positive impact on your immune system. Exercise not only has a preventative effect against cardiovascular disease, but also reduces the risk of inflammatory processes in the entire body. Exercise also helps you to burn excess calories that could otherwise be converted into pro-inflammatory body fat.
- Environmental factors: pollutants in the air, pesticides in food and chemicals in cosmetics can trigger silent inflammation²⁰. It is advisable to use organic products and low-pollutant alternatives to reduce the burden on the body. Avoiding passive smoking and using air purifiers can also help to minimize your exposure to pollutants and reduce silent inflammation.
LPS as a trigger for inflammation
Lipopolysaccharides (LPS) are a major cause of silent inflammation in the body²¹. These bacterial endotoxins, which occur in the cell wall of gram-negative bacteria, can enter the bloodstream during intestinal dysbiosis or infections and upregulate inflammatory factors. This process is known as endotoxinemia.
Even low concentrations of LPS in the blood can trigger a cascade of pro-inflammatory cytokines that lead to chronic inflammation. To minimize the effects of LPS on the body, it is important to address the causes of silent inflammation. A healthy diet rich in anti-inflammatory substances can help. The Mediterranean diet, for example, ensures that the body is supplied with important nutrients that counteract inflammation and even have a positive effect on telomeres²².
Regular exercise and stress reduction are also key to reducing inflammatory factors in the body. Exercise promotes the production of anti-inflammatory cytokines, while stress reduction can reduce the production of pro-inflammatory cytokines. Techniques such as meditation, yoga and breathing exercises can help to reduce stress levels and strengthen the immune system.
It is important to recognize the symptoms of silent inflammation at an early stage and take action. Signs such as fatigue, social withdrawal or listlessness can indicate silent inflammation. If you notice these symptoms, you should consult a doctor to address the causes and promote measures such as a healthy diet, regular exercise and stress reduction.
Pro-inflammatory stimulus and immune balance
A pro-inflammatory stimulus is a signal that stimulates your immune system to start an inflammation. Normally, this is a healthy response to injury or infection. However, in the case of silent inflammation, this stimulus persists and can lead to chronic inflammation. The immune balance, i.e. the balance between pro-inflammatory and anti-inflammatory forces in the body, is crucial here. In the case of silent inflammation, this balance is disturbed, which leads to overactivity of the immune system and chronic inflammation.
The pro-inflammatory cytokines that are released during silent inflammation can increase the activity of the enzyme indoleamine-2,3-dioxygenase (IDO). This leads to a switch in tryptophan metabolism towards kynurenine, which in turn can lead to a serotonin deficiency. The body uses kynurenine and its metabolites to regulate the immune balance. However, in the case of silent inflammation, immunosuppression by kynurenine can contribute to chronic inflammation. It is therefore important to minimize the pro-inflammatory stimuli and restore the immune balance to protect your body's health.
How to recognize silent inflammation
Although silent inflammation is asymptomatic, there are some signs that may indicate it: chronic fatigue, joint pain, digestive problems, depressive moods and unexplained weight gain are a few examples. Another indication of silent inflammation is so-called “gluten sensitivity independent of coeliac disease”. Many people who abstain from gluten report an improvement in their symptoms, even if they have not been diagnosed with classic coeliac disease. This could indicate that the ATIs contained in wheat, not gluten itself, trigger silent inflammation in your body.
Parameters of the silent inflammation check
The silent inflammation check is an important step towards recognizing and reducing the risk of secondary diseases. This check detects low-grade, systemic inflammation, its main trigger - exposure to bacterial LPS - and changes in tryptophan metabolism as a negative consequence of silent inflammation.
hsCRP as a marker for silent inflammation
- The high-sensitivity C-reactive protein (hsCRP) is an important marker for silent inflammation. An elevated hsCRP level can indicate the presence of inflammation in the body, even if there are no obvious symptoms. The hsCRP value is ten times more sensitive than the normal CRP value and can therefore detect silent inflammation even at low inflammation levels. An hsCRP value above 0.56 mg/l indicates silent inflammation and can help you to recognize silent inflammation at an early stage.
- Another important parameter is the LPS value. The main cause of silent inflammation is bacterial lipopolysaccharides (LPS), which constantly enter the bloodstream and thus upregulate inflammatory factors in the body. This constant exposure can lead to a chronic inflammatory reaction.
- Tryptophan metabolism is also a crucial factor. High IDO activity shifts tryptophan metabolism towards kynurenine, which lowers tryptophan levels. This leads to a serotonin deficiency, as tryptophan, the starting material for serotonin synthesis, is missing. A low serotonin level can in turn lead to sleep disorders and depressive moods.
By analyzing these parameters, the silent inflammation check can help you to identify silent inflammation and reduce the risk of chronic diseases. An early diagnosis enables you to take targeted measures and improve your health in the long term.
Actions against silent inflammation
Fortunately, there are many ways in which you can actively combat silent inflammation yourself:
Anti-inflammatory diet
Your diet plays a central role in the fight against silent inflammation. A diet rich in antioxidants and omega-3 fatty acids is recommended. Curcumin in particular, which is contained in turmeric, has been shown to have a strong anti-inflammatory effect.²³ Supplements containing curcumin and other anti-inflammatory substances can support your body in this process. Omega-3 fatty acids, which are found in oily fish, but also in flaxseed, chia seeds, walnuts and oils derived from them, also have strong anti-inflammatory properties.
No wheat and gluten
By reducing gluten and wheat in your diet, you can minimize inflammatory reactions²⁴ in the body. Studies have shown that people with a sensitivity to wheat proteins such as ATIs often benefit from a gluten-free diet. This can be particularly crucial for autoimmune diseases such as Hashimoto's thyroiditis. Gluten-free alternatives offer a way to avoid inflammation-promoting proteins without sacrificing taste.
Stress management
Chronic stress is a major trigger of silent inflammation. Regular relaxation techniques such as meditation, yoga or breathing exercises can lower cortisol levels and reduce the risk of inflammation. Learning mindfulness techniques and consciously reducing stressors in everyday life also play a key role in protecting your body from harmful inflammation.
Movement
Regular physical activity, such as moderate endurance training or weight training, helps you to break down pro-inflammatory fat cells and support heart health. It is important to exercise regularly and in moderation, as excessive exercise can put a strain on the immune system and increase inflammation. Exercise also improves oxygen exchange in the body, which also helps to reduce inflammatory processes.
Essential Oils
Essential oils, such as frankincense, copaiba and chamomile, have strong anti-inflammatory properties. Studies have shown that frankincense oil²⁵ is particularly effective in treating chronic inflammation. With regular use, these oils can help you to regulate inflammatory processes in the body. Frankincense, which has been used in traditional medicine for thousands of years, promotes healing and can relieve chronic inflammation in the long term.
Supplements
In addition to a balanced diet, certain dietary supplements can help to combat silent inflammation. Vitamin D26, omega-3 fatty acids27 and curcumin23 are particularly effective as they support anti-inflammatory processes in the body. Supplements that have been specially developed to promote cell metabolism and have an anti-inflammatory effect can also be considered. Regular supplementation of these vital substances can help you to reduce inflammation-promoting cytokines and strengthen the body in the long term.
Preventing inflammation - minimal effort, great benefit
Silent inflammation is an insidious health risk that often goes unnoticed for a long time. It can lead to serious chronic illnesses if you don't recognize and treat it in time. However, silent inflammation can be successfully combated with a conscious lifestyle that focuses on an anti-inflammatory diet, regular exercise and stress management. Products that support cell metabolism and inflammation regulation offer you a useful supplement to strengthen the body holistically and reduce the risk of chronic inflammation.
This article is based on carefully researched sources:
Sources & bibliography
- Soehnlein O, Libby P , “Targeting inflammation in atherosclerosis - from experimental insights to the clinic,” 2021, Nature Reviews Drug Discovery 20(8): 589-610
- Yeung CHC, Schooling CM , “Systemic inflammatory regulators and risk of Alzheimer's disease: a bidirectional Mendelian-randomization study,” 2021, International Journal of Epidemiology 50(3): 829-840
- Buang N, Strid J , “The IL-33/ST2 axis and tissue Treg maintains epithelial homeostasis in the skin and restrains cancer development,” 2024, GEO Accession GSE241061
- Alsaigh T, Torkamani A , “Decoding the transcriptome of calcified atherosclerotic plaque at single-cell resolution,” 2020, GEO Accession GSE159677
- Santos AS et al. , “Inflammatory pathways in peripheral blood expression profile of recent-onset type 1 diabetes,” 2022, GEO Accession GSE151835
- Korsunsky I et al. , “Cross-tissue, single-cell stromal atlas identifies shared pathological fibroblast phenotypes in four chronic inflammatory diseases,” 2022, GEO Accession GSE185711
- Parisien M et al. , “Mouse transcriptomics reveals extracellular matrix organization as a major pathway involved in inflammatory and neuropathic pain,” 2019, GEO Accession GSE111216
- Ziegler KA et al. , “Single-nucleus RNA-seq of healthy (sham) and heart diseased (TAC) SCGs,” 2023, GEO Accession GSE231765
- Stockinger B et al. , “Environmental factors transmitted by aryl hydrocarbon receptor influence severity of psoriatic skin inflammation”, 2014, GEO Accession GSE47944
- Ricker MA, Haas WC , “Anti-Inflammatory Diet in Clinical Practice: A Review”, 2017, Nutr Clin Pract 32(3): 318-325, doi: 10.1177/0884533617700353. PMID: 28350517
- Zhang N, Wang
- Nishimura S et al. , “CD8+ effector T cells contribute to macrophage recruitment and adipose tissue inflammation in obesity” 2009, Nature Medicine 15: 914-9
- Feuerer M et al., “Lean, but not obese, fat is enriched for a unique population of regulatory T clls that affect metabolic parameters,” Nature Medicine 2009, 15: 930-939, Doi:10.1038/nm.2002
- Zevallos VF, Yogev N, Hauptmann J, Nikolaev A, et al. , “Dietary wheat amylase trypsin inhibitors exacerbate CNS inflammation in experimental multiple sclerosis”, 2023, Gut 73(1): 92-104, doi: 10.1136/gutjnl-2023-329562
- Reig-Otero Y, Mañes J, Manyes L , “Amylase-Trypsin Inhibitors in Wheat and Other Cereals as Potential Activators of the Effects of Nonceliac Gluten Sensitivity,” 2018, Journal of Medicinal Food 21(3): 207-214, doi: 10.1089/jmf.2017.0018
- Zhang B et al. , “Single cell RNA-seq for PBMC from rheumatoid arthritis patient,” 2020, GEO Accession GSE159117
- Thaiss CA et al. , “The enteric nervous system relays psychological stress to intestinal inflammation,” 2023, GEO Accession GSE229320
- Erquan Zhang et al. , “Prolonged sleep deprivation induces cytokine storm-like syndrome in mammals,” 2023, GEO Accession GSE213497
- Liu L, Rando T , “Exercise reprograms the inflammatory landscape of multiple stem cell compartments during mammalian aging III,” 2023, GEO Accession GSE196359
- Liu Z, Lu Y , Zhong K, Wang C, Xu doi: 10.1016/j.ecoenv.2022.113382
- Van Looveren K, Timmermans S, Vandewalle J, Libert C , “Lipopolysaccharide induced inflammatory response in mouse intestinal epithelial cells,” 2020, GEO Accession GSE139903
- Davinelli S, Trichopoulou A, Corbi G, De Vivo I, Scapagnini G , “The potential nutrigeroprotective role of Mediterranean diet and its functional components on telomere length dynamics,” 2018, Aging Research Reviews . doi: 10.1016/j.arr.2018.11.001. PMID: 30448616
- Jazayeri-Tehrani, M. , Belcaro, G. , Barnes, PJ , & Brennan, P. (2020). Curcumin: A modulator of inflammatory signaling pathways in the immune system. Inflammopharmacology
- Nichols, H. (Year). Wheat proteins may cause inflammation beyond the gut. MedicalExpress .
- Siddiqui MZ, "Boswellia serrata, a potential anti-inflammatory agent: an overview.", Indian J Pharm Sci. 2011 May, Indian J Pharm Sci. 2011
- Ao, T. , Kikuta, J. , & Ishii, M. (2021). The effects of vitamin D on immune system and inflammatory diseases. Biomolecules , 11(11), 1624
- Mildenberger, J., Johansson, I., Sergin, I., Kjøbli, E., Damås, JK, Razani, B., Flo, TH, & Bjørkøy, G. (2017). N-3 PUFAs induce inflammatory tolerance by formation of KEAP1-containing SQSTM1/p62-bodies and activation of NFE2L2. Autophagy