Themen dieses Blogartikels:
Table of contents
- What is the gut-brain axis?
- Why is the gut-brain axis so important to you?
- The scientific basis: How communication works
- When the gut-brain axis gets out of sync
- How to strengthen your gut-brain axis
- Intestinal bacteria & neurotransmitters: An unbeatable team
- Gut-brain axis and diseases: From irritable bowel syndrome to depression
- Conclusion
- Sources & Bibliography
What is the gut-brain axis?
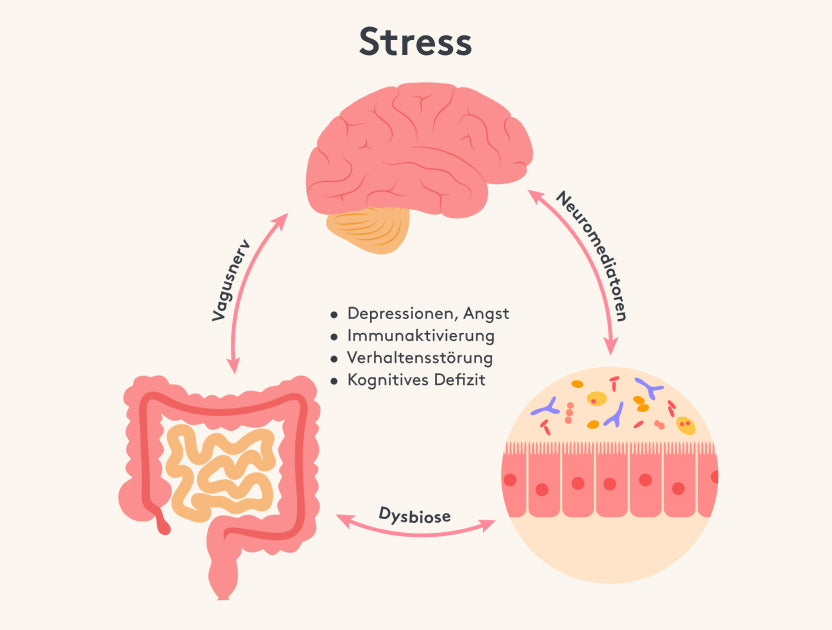
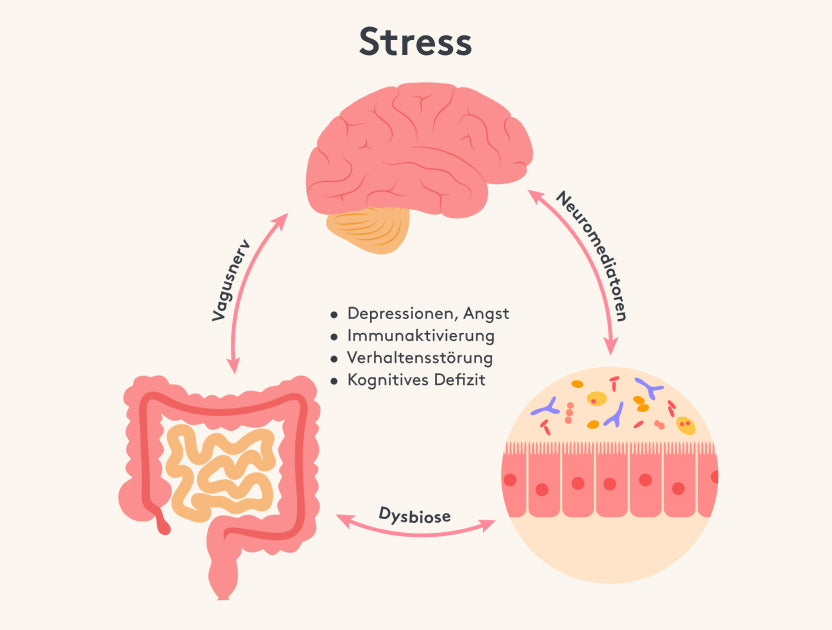
Imagine your body as a sophisticated network in which all systems communicate with each other. The gut-brain axis is a bidirectional communication pathway between your gastrointestinal tract and your central nervous system (i.e. brain and spinal cord).² This communication is not only purely nervous in nature, but also includes hormonal and immunological signals. All this means that your gut “talks” to your brain - and vice versa. This can affect both your physical and mental health.³
1.1. The role of the enteric nervous system
You may have heard the term "gut brain" before. This refers to the so-called enteric nervous system (ENS), which is located in the intestines. It consists of a dense network of neurons that is comparable in complexity to the brain itself.⁴ The ENS is responsible for controlling digestion and can even regulate many processes independently of the brain. Nevertheless, it constantly exchanges signals with the central nervous system. This constant communication is the reason why we possess a veritable "gut intelligence."
1.2. Microbiome: The secret superpower
In addition to the ENS, the gut microbiome—the community of microorganisms living in the gut—plays a key role in the gut-brain axis.⁵ The bacteria, viruses, and fungi that live in your gut are responsible for much more than just digesting food. They produce vitamins, support your immune system, and create messengers that can reach your brain directly or indirectly. When your microbiome is healthy, your entire body generally benefits. However, when the microbiome becomes unbalanced, it can affect your mood, your ability to concentrate, and your overall health.⁶
2. Why is the gut-brain axis so important to you?
One of the main branches of communication between the brain and the intestines is the so-called vagus nerve. This is composed of 80% afferent, or influx, fibers and 20% efferent, or efferent, fibers2. The difference between the fibers is that afferent nerves transport signals from the body to the nerve cells, whereas efferent nerves act in the opposite way. Through this process, metabolic products are ultimately sent from the gut toward the central nervous system, from where they are transmitted to the appropriate nerve pathways.


2.1. Mood and mental health
Have you noticed that an uneasy gut feeling is often accompanied by a bad mood or even anxiety? Researchers have discovered that gut bacteria can influence important neurotransmitters such as serotonin and dopamine⁷. Serotonin, also known as the "happy hormone," plays a key role in your mood. A healthy gut can therefore help you feel more content and balanced. Gut health therefore also has a direct impact on your psyche, as nutrients and microorganisms in the gut can influence emotions and cognitive abilities.
Interestingly, about 90 percent of the body's serotonin is produced in the gut, not the brain.⁷ So if you suffer from persistent low mood, it might be worth taking a look at your digestive system.
2.2. Stress resistance and sleep quality
You might be asking yourself: “Why should I bother? My gut is just working away anyway.” The answer is: because your gut health is much more closely linked to your mental state than has long been assumed. The gut-brain axis has a direct impact on your emotions, your stress levels and even on the development of various diseases. The interactions between the gut and the brain are particularly important with regard to neurological diseases such as Parkinson's and Alzheimer's, as they expand our understanding of these diseases and the role of the brain in the gut-brain axis.
2.3. Immune system and inflammation
Did you know that around 70 percent of your immune system is located in your gut?¹⁰ This highlights how important a balanced gut flora is for your defenses. If your gut microbiome becomes imbalanced—for example, due to an unbalanced diet, medication, or chronic stress—your immune system can become permanently irritated. This imbalance promotes inflammatory processes in the body, which in turn can affect your brain. Chronic inflammation is associated with a variety of diseases, including those affecting the nervous system¹¹.
3. The scientific basis: How communication between gut and brain works
To understand exactly how your gut and your brain communicate with each other, it's worth taking a quick look behind the scenes.
3.1 Neural communication via the vagus nerve
The vagus nerve is the most important nerve that connects the gut directly to the brain.¹² As a vital organ in the gut-brain axis, the gut plays a central role in well-being and health. It transmits signals about bowel movements, levels of fullness, and even pain sensations to the brain. Conversely, the brain sends signals to the gut to control digestive processes. Smooth vagus nerve activity is therefore essential for a balanced organism.
3.2. Hormonal signals
Another way of communication is through neurotransmitters. Researchers have discovered that intestinal bacteria produce neurotransmitters, but can also influence them and thus use them as signaling pathways. Well-known examples include histamine, steroids, and gasotransmitters3.
3.3 Immunological interaction
As already mentioned, the immune system also plays a major role. Gut bacteria can activate or inhibit parts of your immune system. The causal relationships between the microbiome and various diseases, especially neurological and mental disorders, are complex and require interdisciplinary research to gain a better understanding of these dynamic interactions. If certain substances cross the intestinal barrier into the bloodstream, they can penetrate the brain.¹⁴ If the intestinal barrier is permeable (leaky gut), unwanted substances can reach the brain and promote inflammatory processes there.
Why is the gut-brain axis so important?
Also in terms of general health, the communication between the intestine and the brain has relevant tasks. The intestine alone is one of the most important organs of the human body. On the one hand, almost all microorganisms in the human body are located there. On the other hand, almost all immune cells of the human body are also located there. In order to protect the body from pathogens, it is advisable to promote the diversity of intestinal bacteria through diet. Because as we know, it is mainly the intestine that sends most of the signals to the brain. If this is now impaired due to poor nutrition, genetic changes or pathogens, this also has a negative impact on our cognitive performance.
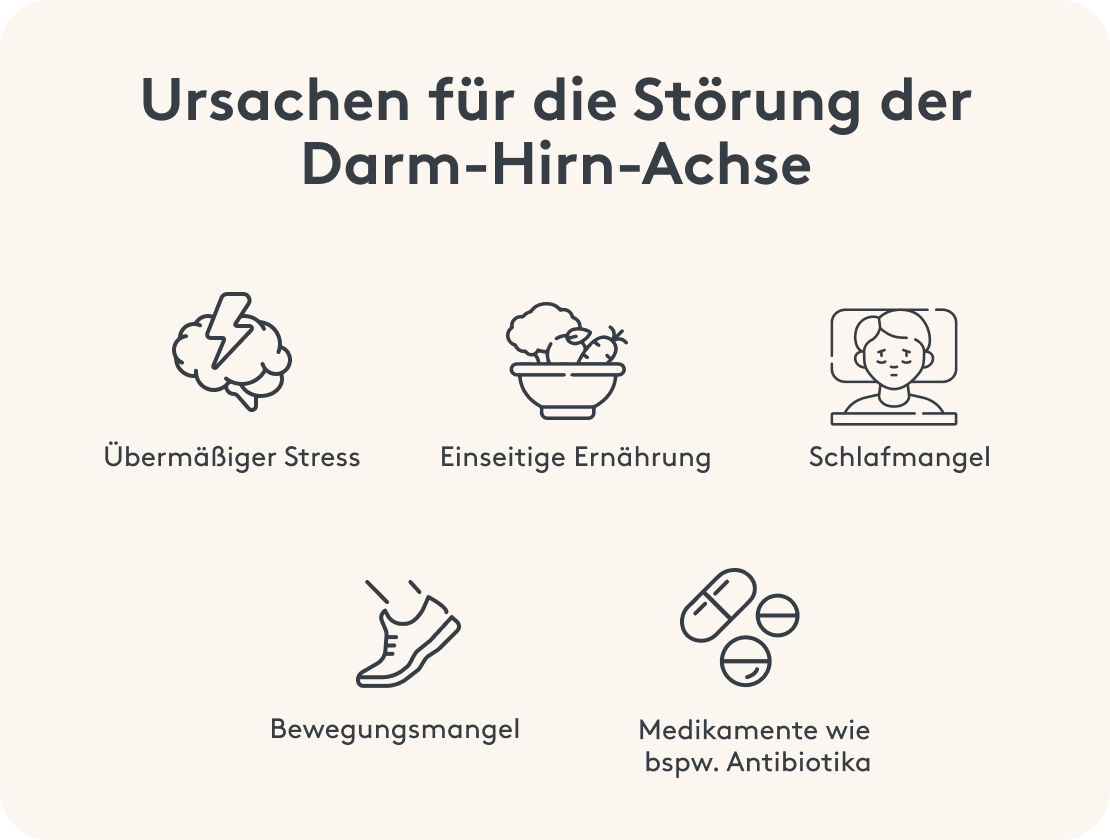
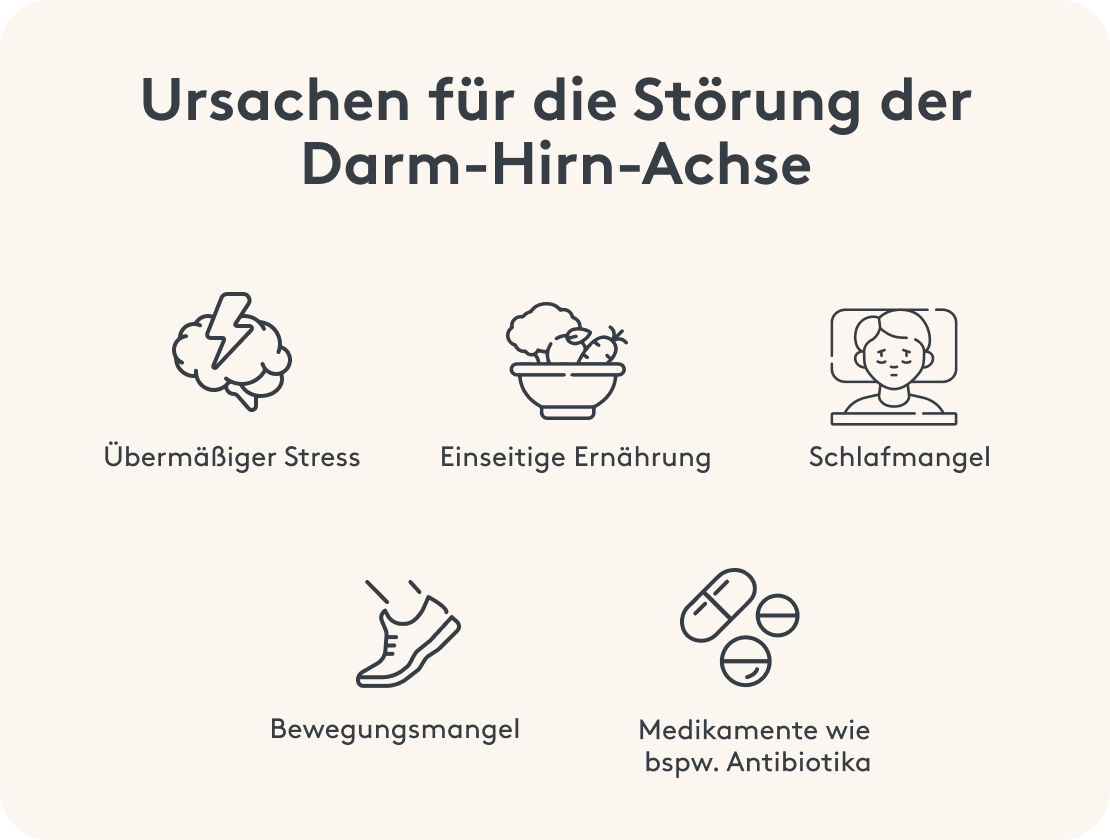
4.1. Causes of imbalances
- Unbalanced diet: Fast food, high-sugar foods and processed products can unbalance your microbiome¹⁵.
- Excessive stress: Chronic stress affects the hormonal and nervous system, which also has an impact on the gut.
- Medication: Antibiotics kill not only harmful but also beneficial bacteria, which throws the intestinal flora out of balance.
- Lack of sleep: Too little or poor sleep impairs the regeneration processes, which also include the maintenance of healthy intestinal flora.
4.2. Possible consequences
A disrupted gut-brain axis can manifest itself in a variety of ways. Changes in the function of one of these organs can have significant effects on the other, as both the gut and the brain are vital organs that communicate intensively and are interconnected via the gut-brain axis. Some people notice more digestive problems such as bloating, fullness, or diarrhea, while others complain of irritability, restlessness, and mood swings.1⁶ Symptoms such as fatigue or difficulty concentrating are also frequently reported. In the long term, the risk of diseases such as irritable bowel syndrome, chronic inflammatory bowel disease, or even mental disorders increases.
5. How to strengthen your gut-brain axis
Fortunately, you have a lot of control over whether your gut and brain work together harmoniously. With a few targeted measures, you can nurture your microbiome and thus contribute to your overall health.
5.1. Eat probiotic and prebiotic foods
A proven strategy is the regular consumption of probiotic and prebiotic foods¹⁷.
- Probiotics : These are foods that contain live microorganisms (usually bacteria) that support your gut flora. These include fermented products such as yogurt, kefir, sauerkraut, or kombucha.
- Prebiotics : These are fibers that serve as "food" for your gut bacteria. They can be found in foods like oatmeal, flaxseed, onions, leeks, garlic, and chicory.
Try to include these products in your diet regularly. Pay attention to quality: When it comes to fermented products like sauerkraut, make sure they haven't been pasteurized, as this will destroy many beneficial bacteria.
5.2. Reduce stress and learn relaxation techniques
Because stress is one of the main causes of a disrupted gut-brain axis, it's worth incorporating relaxation techniques into your daily routine.¹⁸ Meditation, yoga, autogenic training, or simply a long walk in nature often work wonders. Even a few minutes a day can help reduce your stress levels and thus relieve your gut.
The vagus nerve can be activated through breathing exercises and mindfulness practices, which increases your heart rate variability and makes you more resilient to stress overall.¹² Be aware that inner calm benefits not only your head but also your gut.
5.3. Pay attention to sleep and regeneration
Sleep is much more than just "doing nothing." Numerous repair and regeneration processes take place in your body at night, which also benefit your digestive tract.¹⁹ Aim to get seven to eight hours of sleep each night. A regular sleep routine—going to bed and waking up at the same time every night, if possible—can help stabilize your circadian rhythm. Good sleep hygiene ensures your microbiome remains intact and supports your immune system.
5.4. Focus on a healthy lifestyle
In addition to a balanced diet and relaxation, a healthy lifestyle also includes sufficient exercise. Just 30 minutes of moderate activity a day (such as brisk walking, cycling, or swimming) can promote your gut activity and thus microbiome health.²⁰ If you smoke, keep in mind that nicotine and other harmful substances can irritate your gut and negatively impact the environment. Excessive alcohol consumption also negatively impacts your gut flora.
6. Gut bacteria and neurotransmitters: An unbeatable team
As already mentioned, some gut bacteria are capable of producing neurotransmitters such as serotonin, dopamine, and GABA.⁵ These messenger substances play a crucial role in your emotional balance and cognitive performance.
6.1. Serotonin: Your happiness hormone
When you hear the word serotonin, you usually think of happiness and contentment. However, about 90 percent of the serotonin in your body is produced in the gut, which once again underscores the importance of gut health.⁷ Current research suggests that changes in the microbiome and disrupted gut-brain communication play a major role. Experts like Prof. Holzer are investigating the importance of the gut-brain axis in irritable bowel syndrome and highlighting the effects of stress on both organs.
A serotonin deficiency can lead to depression, sleep problems, and a general imbalance. A healthy gut therefore indirectly contributes to a stable state of mind.
6.2. Dopamine: Motivation and Drive
Dopamine is the neurotransmitter responsible for drive, motivation, and the feeling of reward. When you feel good after completing a task, dopamine is usually involved. Certain gut bacteria can also be involved in dopamine production.²⁴ While the majority of your dopamine is produced in the brain, a healthy gut flora can positively influence your entire metabolism, making more dopamine available.
6.3. GABA: The calming center
GABA (gamma-aminobutyric acid) is an inhibitory neurotransmitter that helps us reduce stress and inner restlessness. A deficiency in GABA is associated with anxiety and sleep problems. Some studies suggest that certain probiotic strains can influence GABA concentrations.²⁵ This demonstrates how directly our gut inhabitants can influence our emotions.
Initial research results show that the gut microbiome can also play a role in the development of such diseases, for example through chronic systemic inflammation or the formation of certain proteinaceous deposits that can travel from the gut to the brain. The Else Kröner-Fresenius Foundation supports interdisciplinary research on the gut-brain axis and its connection to neurological diseases, particularly through funding the Clinician Scientist Program, which provides young researchers with the opportunity to explore cross-cutting topics while receiving support from the foundation.
7. Gut-brain axis and diseases: From irritable bowel syndrome to depression
The gut-brain axis plays a crucial role in the development or progression of various diseases. Understanding how closely intertwined the two systems is also a great way to appreciate how important it is to maintain this balance.
7.1 Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome is characterized by chronic digestive symptoms such as diarrhea, constipation, bloating, or pain. Many sufferers also report feelings of anxiety, depression, or general exhaustion.²⁶ Current research suggests that changes in the microbiome and disrupted gut-brain communication play a major role. Therapy that also focuses on the intestinal flora (e.g., through probiotics and nutritional therapy) often shows good results.
7.2. Depression and anxiety disorders
For a long time, depression was considered exclusively a brain-centered disorder. It is now clear that the gut microbiome and inflammatory processes can contribute significantly to the development of this disease.⁷ A disrupted gut-brain axis can lead to reduced availability of serotonin and other positive neurotransmitters. Anxiety disorders are also increasingly being linked to the state of the gut flora.
7.3. Neurodegenerative diseases
Diseases such as Parkinson's or Alzheimer's are often associated with inflammatory processes in the brain.²⁷ Initial research results show that the gut microbiome can also play a role in the development of such diseases, for example through chronic systemic inflammation or the formation of certain proteinaceous deposits that can travel from the gut to the brain. Although much more research is needed, it is becoming clear how central gut health can be to overall brain health.
Support by MITOcare
This article is based on carefully researched sources:
Sources & bibliography
- Mayer EA et al. (2015): Gut microbes and the brain: Paradigm shift in neuroscience. J. Neurosci. 35(41): 13860-13867.
- Carabotti M et al. (2015): The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 28(2): 203-209.
- Cryan JF et al. (2019): The Microbiota-Gut-Brain Axis. Physiol. Rev. 99(4): 1877-2013.
- Collins SM et al. (2012): The interplay between the intestinal microbiota and the brain. Nat Rev Microbiol. 10(11): 735-742.
- Sharon G et al. (2016): Specialized metabolite production by gut microbiota in synergy with the host can shape immune and metabolic outcomes. Cell. 167(7): 1897-1906.
- Hills RD Jr et al. (2019): Gut Microbiome: Profound Implications for Diet and Disease. Nutrients. 11(7): 1613.
- Strandwitz P (2018): Neurotransmitter modulation by the gut microbiota. Brain Res. 1693(Pt B): 128-133.
- Rea K et al. (2016): The Stress Microbiota Interface: Psychological and Biological Consequences for the Human Microbiota. Curr Opin Behav Sci. 9: 105-110.
- Benedict C et al. (2016): Gut Microbiota and Sleep. Sleep Med Clin. 11(4): 463-468.
- Hooper LV et al. (2012): Interactions between the microbiota and the immune system. Science. 336(6086): 1268-1273.
- Libby P (2007): Inflammatory mechanisms: the molecular basis of inflammation and disease. Nutr Rev. 65(12 Pt 2): S140-S146.
- Breit S et al. (2018): Vagus Nerve as Modulator of the Brain-Gut Axis in Psychiatric and Inflammatory Disorders. Front Psychiatry. 9: 44.
- Murphy KG, Bloom SR (2006): Gut hormones and the regulation of energy homeostasis. Nature. 444(7121): 854-859.
- Braniste V et al. (2014): The gut microbiota influences blood-brain barrier permeability in mice. Sci Transl Med. 6(263): 263ra158.
- Jang HM et al. (2020): High dietary fat intake increases susceptibility to gut inflammation and colitis. Cell Host Microbe. 27(2): 212-224.
- El-Salhy M et al. (2019): The possible role of the gut microbiota in the development and progression of chronic fatigue syndrome. Metabolites. 9(7): 162.
- Sanders ME et al. (2019): Probiotics and prebiotics: prospects for public health and nutritional recommendations. Ann N Y Acad Sci. 1441(1): 19-28.
- Guarner F et al. (2012): The effect of fermentation products and their in vivo effects. J Clin
- Sun J et al. (2024): Metabolic disruption exacerbates intestinal damage during sleep deprivation by abolishing HIF1α-mediated repair. Cell Reports. 114915.
- Yang W et al. (2021): Moderate-Intensity Physical Exercise Affects the Exercise Performance and Gut
- Microbiota of Mice. Front Cell Infect Microbiol. 11:712381.
Strandwitz P (2018): Neurotransmitter modulation by the gut microbiota. Brain Res. 1693(Pt B):128-133. - Yano JM et al. (2015): Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell. 161(2):264-276.
- O'Mahony SM et al. (2015): Serotonin, tryptophan metabolism and the brain-gut-microbiome axis. Behav Brain Res. 277:32-48.
- Strandwitz P (2018): Neurotransmitter modulation by the gut microbiota. Brain Res. 1693(Pt B):128-133.
- Barrett E et al. (2012): γ-Aminobutyric acid production by culturable bacteria from the human intestine. J Appl Microbiol. 113(2):411-417.
- Fond G et al. (2014): Anxiety and depression comorbidities in irritable bowel syndrome (IBS): a systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci. 264(8):651-660.
- Rudzki L, Maes M (2020): The Microbiota-Gut-Immune-Glia (MGIG) Axis in Major Depression. Mol Neurobiol. 57(10):4269-4295.
- Stephenson J et al. (2018): Inflammation in CNS neurodegenerative diseases. Immunology. 154(2):204-219.